[ad_1]
Healthcare Payment Learning and Action Network (local area network) Committed to transforming the healthcare system from a quantity-based, service-based reimbursement to an alternative payment model (APM). Although there are a large number of different types of APM, in general, all of them transfer more financial risk to the provider, while also linking reimbursement to the quality of care. In fact, the goal of HCP LAN is to make 100% of the reimbursement of traditional medical insurance and medical insurance advantages belong to the bilateral risk APM, and 50% of the commercial and medical assistance reimbursement belong to the bilateral risk APM by 2025.
HCP LAN defines APM as one of the following four types:
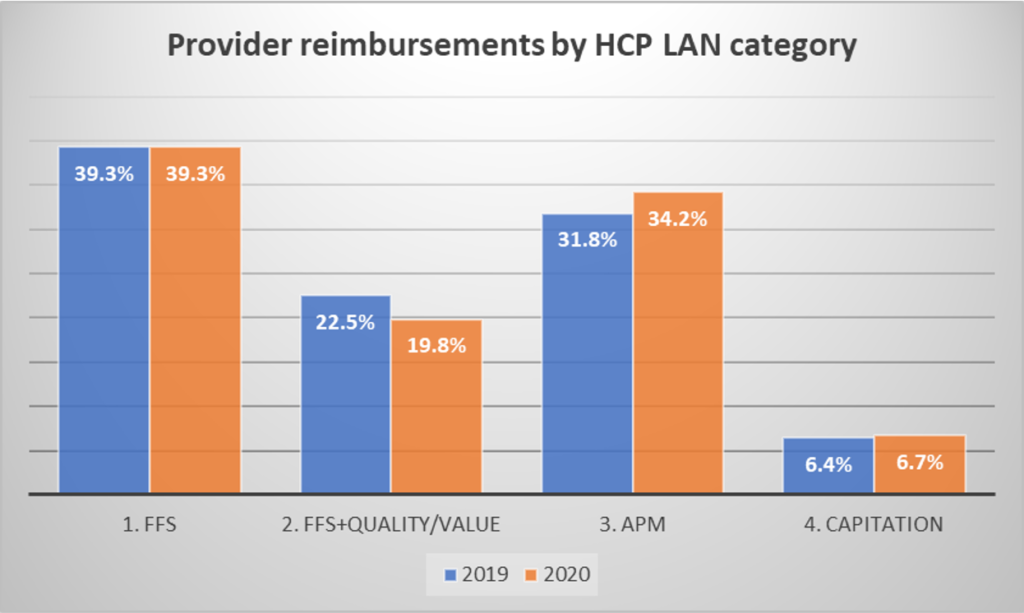
In their 2020-2021 report, APM Measurement: Progress in Alternative Payment Models, HCP LAN uses 2019 and 2020 data to test whether APM is gaining market share. From 2019 to 2020, we did see some shifts to more APM and per capita payments, but FFS payments remained stable at 39.3% of reimbursement. Since 2020 was the peak of the COVID-19 pandemic, it is not surprising that the reimbursement structure has not changed much.
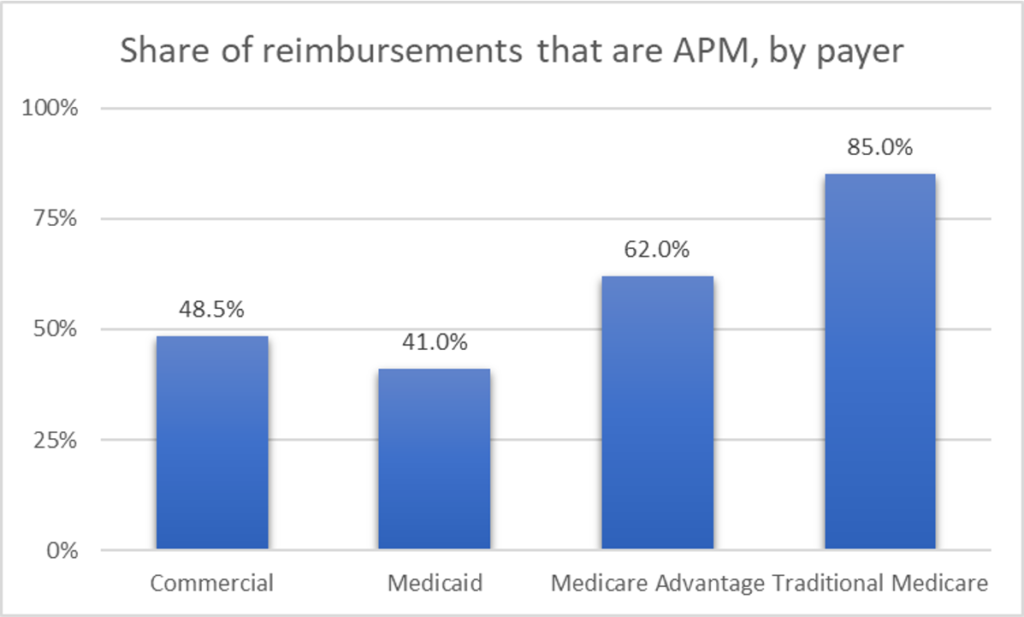
The usage rate of APM also varies depending on the type of payer. Traditional medical insurance has the highest APM usage rate (ie, reimbursement in HCP LAN category 2, 3, or 4), and commercial insurance has the lowest usage rate (see figure below). Please note that with the exception of Medicare Advantage where 21.8% of payments are made through global per-person payments, global per-person payments for most payers (3%-6%) are quite rare.
HCP LAN also conducted a survey of payers and found that 87% of people believe that APM activities will increase in the future. The most interesting are the bundled payment (47%) and shared savings (21%) APM types. It is worth noting that approximately half (44%) of respondents believe that APM will increase supplier integration.
Although payers are excited about the increased financial certainty brought about by APM, suppliers have concerns. The three major challenges in implementing APM are:
- Willingness of providers to take financial risks
- Supplier’s ability to implement APM
- Provider’s interest/preparation
APM has many obvious attractive features, but there are also challenges. Obviously, linking reimbursement to the quality and value of care is a laudable goal. However, in a static environment where the expected results and costs are known with reasonable certainty, it is easiest to estimate value. Due to COVID-19, due to the direct cost of COVID-19 and its impact on the treatment of other diseases, there is great uncertainty in the cost. There is no doubt that the global pandemic makes the implementation of APM challenging. Similarly, as new therapeutic innovations enter the market, quality may improve, but costs may also increase; as the treatment paradigm shifts, values—and the corresponding APM structure—may need to evolve over time .
[ad_2]
Source link








